Title in English: Non-canonical manifestations of FMF in homozygous M694V MEFV genotype: Insights from a large patient cohort
First author: Eitan Giat
Journal: Seminars in Arthritis and Rheumatism
Link to PubMed : https://pubmed.ncbi.nlm.nih.gov/40902213/
Summary by: Dr Catherine Grandpeix-Guyodo

Introduction:
Familial Mediterranean Fever (FMF) is the most common monogenic autoinflammatory disease worldwide. Among the MEFV gene mutations associated with a classic FMF phenotype, homozygous M694V variants are classically associated with the most severe forms of the disease, with more frequent attacks, more frequent arthritis, lower limb pain during exercise, poorer quality of life, higher colchicine requirements, poorer treatment response, and increased risk of inflammatory amyloidosis, with half of AA amyloidosis cases in FMF patients being associated with a homozygous M694V genotype. This study examined clinical and biological manifestations other than those already known, associated with homozygous M694V mutations in a large cohort of patients in Israel.
Patients and methods:
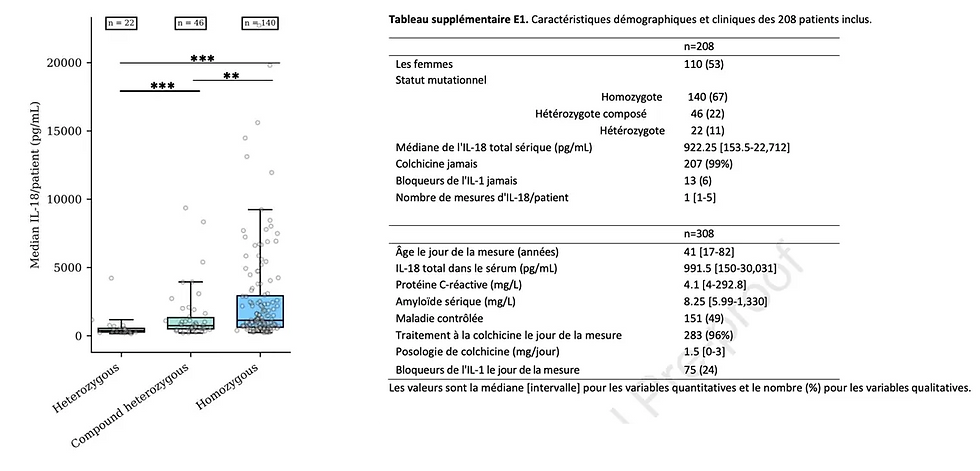
This was a retrospective study of adults with FMF followed between 2010 and 2020 at an Israeli hospital center. Patients carrying the homozygous M694V mutation were compared to a control group of patients with a classic FMF phenotype and either homozygous MEFV mutations other than M694V, compound heterozygotes, or heterozygotes (known variants associated with classic FMF but also presence of variants of unknown significance (VUS) such as E148Q, K695R, P369S).
Results:
The cohort included 3,866 FMF patients, 47.6% male, and 517 (13.4%) homozygous M694V. Significant differences between the two groups were, in homozygous M694V: higher colchicine dosage (median 2 mg/day versus 1.5 mg/day) despite better compliance, greater number of colchicine failures requiring addition of biotherapy (anti-IL1 or anti-TNF) (30% versus 4.2%), higher number of associated pathologies (*ankylosing spondylitis (AS), Behçet's disease, congestive heart failure, deep vein thromboses, chronic renal failure, and hepatic dysfunctions*), more significant abnormalities in biological parameters (CRP, ESR, liver enzymes, bilirubin, creatinine, and uric acid), higher number of hospitalizations and emergency room visits, particularly due to FMF attacks.
The results are the same if patients with at least one M694V mutation are excluded from the control group. Moreover, comparison of a heterozygous M694V group to other controls shows no difference.
It should also be noted that homozygous M694V patients on biotherapies had more AS, Behçet's disease, chronic renal failure, hepatic cytolysis, hyperuricemia, emergency room visits, and hospitalizations. However, there was no difference in terms of cardiovascular pathologies between homozygotes on biotherapies and those on colchicine alone.
Discussion:
In addition to what is described in the literature (more severe phenotype, more attacks, specific locations of FMF flares, poorer response to colchicine, more associations with inflammatory diseases, more AA amyloidosis and chronic renal failure), this study shows in FMF patients with homozygous M694V mutation the use of higher colchicine dosages, more frequent use of biotherapies, no increase in ischemic cardiovascular pathologies despite greater inflammation (possibly due to the action of anti-IL1). The study did find a higher rate of congestive heart failure which could be attributed to greater systemic inflammation, as has been shown in rheumatoid arthritis, Crohn's disease, and ulcerative colitis. The same applies to the higher frequency of deep vein thromboses.
Hepatic dysfunctions and hepatic cytolysis were more frequent in homozygous M694V FMF patients and could also be attributed to systemic inflammation that would generate hepatic steatosis.
To better understand the pathophysiological mechanisms, more studies seem necessary.
Conclusion:
In addition to the more severe and complicated presentations of classic FMF associated with the homozygous M694V genotype of MEFV, higher colchicine requirements or even recourse to biotherapies are observed, more frequent associated pathologies such as inflammatory diseases (AS, Behçet), increased frequency of congestive heart failure, deep vein thromboses, chronic renal failure, and liver diseases. Increased biannual monitoring of homozygous M694V patients seems essential.